2 min read
Do I Need Postoperative Hormonal Suppression?
Restore Center For Endometriosis April 23, 2024

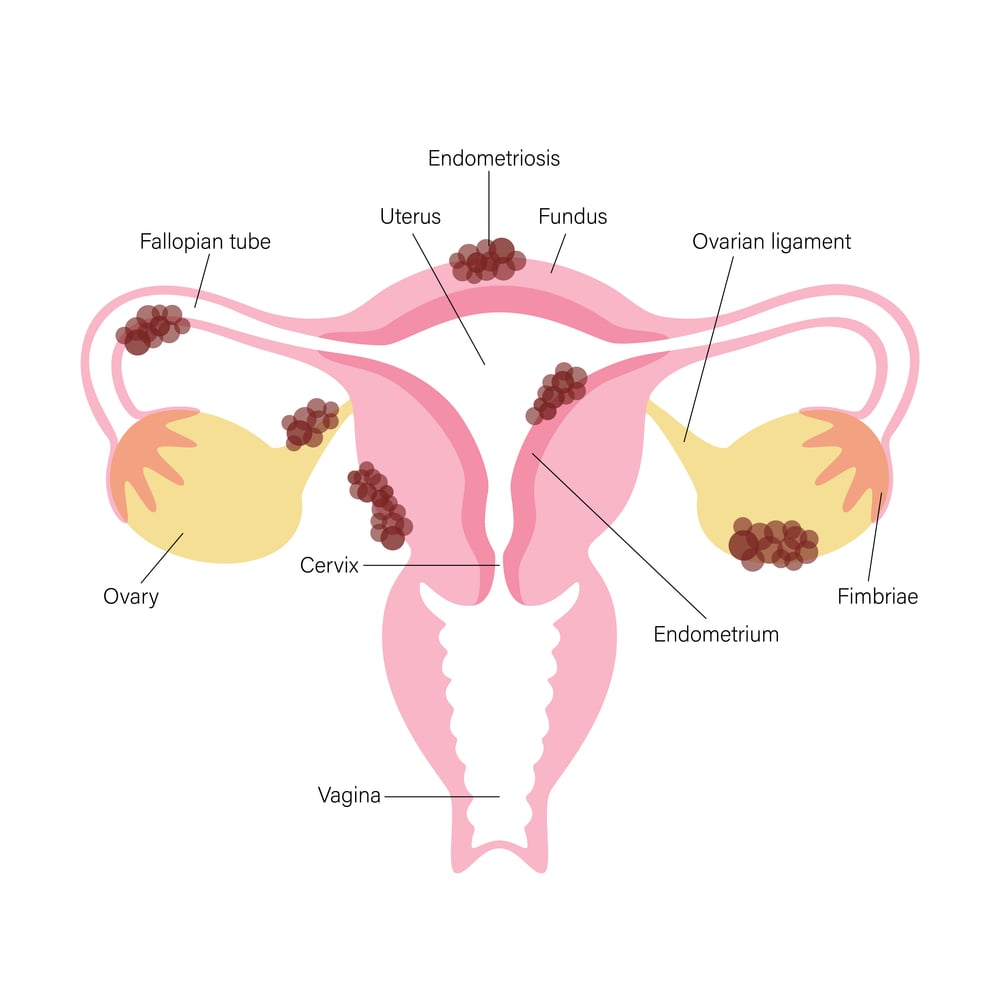
If you’ve researched treatment options for endometriosis, you’re probably wondering, “Do I need postoperative hormonal suppression?”
It’s a common concern, and you’re not alone in asking this question.
Many doctors recommend hormonal suppression therapy after surgery in order to reduce the risk of disease recurrence and to manage pain. It’s also often used for women who are looking to preserve or improve fertility.
However, if the desired result is to enhance fertility, postoperative hormonal suppression is something that should be carefully considered. Studies show that the treatment with hormonal suppression comes with the risks of delaying conception, without a proven benefit on later fertility.
While the reasons for hormonal suppression being prescribed vary, the type of surgery performed determines if this postoperative therapy is needed at all.
Optimal Excision by LAPEX
Optimal Excision by LAPEX (Laparoscopic Excision) surgery is a minimally invasive procedure aimed at completely removing endometrial lesions and affected tissues. Unlike other surgical techniques, Optimal Excision targets the root cause of endometriosis with the goal of completely removing it, offering patients a chance at long-term relief by eradicating the disease rather than merely alleviating symptoms.
With the disease removed, Optimal Excision allows your body to restore your natural fertility, without the use of medications or IVF.
And with just a 2.5% rate of repeat surgery in 10 years, it is highly effective on its own at reducing the risk of the endometriosis recurring or progressing, with the potential for one-and-done surgery.
The Controversy Surrounding Postoperative Hormonal Suppression
Despite the success of LAPEX surgery in addressing endometriosis at its source, the necessity of postoperative hormonal suppression remains a subject of debate.
While hormonal therapies such as oral contraceptives, GnRH agonists, and progestins can effectively reduce pain and delay disease progression, they come with potential side effects and limitations.
For example, studies show they have limited to no impact on increasing chances of pregnancy, and postoperative hormonal suppression may actually delay conception.
Additionally, some experts argue that since Optimal Excision surgery removes the underlying tissue causing endometriosis, hormonal suppression may not be essential for long-term management of the disease, either.
Alternative Postoperative Pain Management Strategies
Hormonal suppression therapy is not the only option to manage pain post-surgery. Other viable pain management strategies include the following:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs like ibuprofen and naproxen can effectively reduce inflammation and alleviate pain associated with endometriosis.
Dietary Changes
Certain dietary modifications also can help reduce inflammation and manage endometriosis symptoms. Incorporating anti-inflammatory foods such as fruits, vegetables, whole grains, and omega-3 fatty acids while limiting processed foods, red meat, and high-fat dairy products may provide relief.
Consider the Anti-Inflammatory and Elimination Diet for Adults Living with Endometriosis developed at Saint Louis University in conjunction with Dr. Yeung, as an example of using diet as a way to manage inflammation and associated pain.
Physical Therapy
Pelvic floor physical therapy can help relieve pelvic pain and improve muscle function, providing long-term benefits for individuals with endometriosis.
Acupuncture and Mind-Body Techniques
Practices like acupuncture, yoga, and meditation have shown promise in reducing pain and improving overall well-being in individuals with endometriosis.
Functional Medicine and Supplements
This is a rapidly growing field with the potential to change the landscape of options for patients with inflammation and certain mineral, vitamin or nutritional deficiencies through personalized evaluation and supplementation.
The Importance of Individualized Treatment
Ultimately, the decision regarding postoperative hormonal suppression should be based on individual preferences, disease severity, and treatment goals. While hormonal therapy may be appropriate for some patients and in some situations, others may find relief through non-hormonal approaches.
With advancements in surgical techniques and alternative pain management strategies, you have more choices than ever before when it comes to managing your endometriosis symptoms and preventing disease recurrence or progression.
And if your goal is improving fertility, you definitely want to balance potential benefits of hormonal treatment with any risky side effects.
Consulting with an experienced specialist at RESTORE Center for Endometriosis can help you explore your options and develop a personalized treatment plan tailored to your needs.
Click here to schedule a consultation with Dr. Yeung to discuss the best approach for your unique needs.
Related Posts