3 min read
What Are Adhesions and How Are They Treated?
Restore Center For Endometriosis April 23, 2024
Dr. Yeung has a wealth of experience in effectively treating patients grappling with severe adhesions. For many, the surgeries performed have not just been transformative but lifesaving. Our commitment to post-operative care extends equally to our adhesion patients as it does to those with endometriosis.
What are Adhesions?
Adhesions are bands of scar tissue that form between neighboring organs and structures, causing them to adhere together. Adhesions can vary in texture, ranging from delicate, cobweb-like strands to dense, glue-like masses. They may develop due to various factors such as disease (like endometriosis), infection (such as pelvic inflammatory disease), injury (often following abdominal surgery), or even for reasons unknown (referred to as idiopathic adhesions).
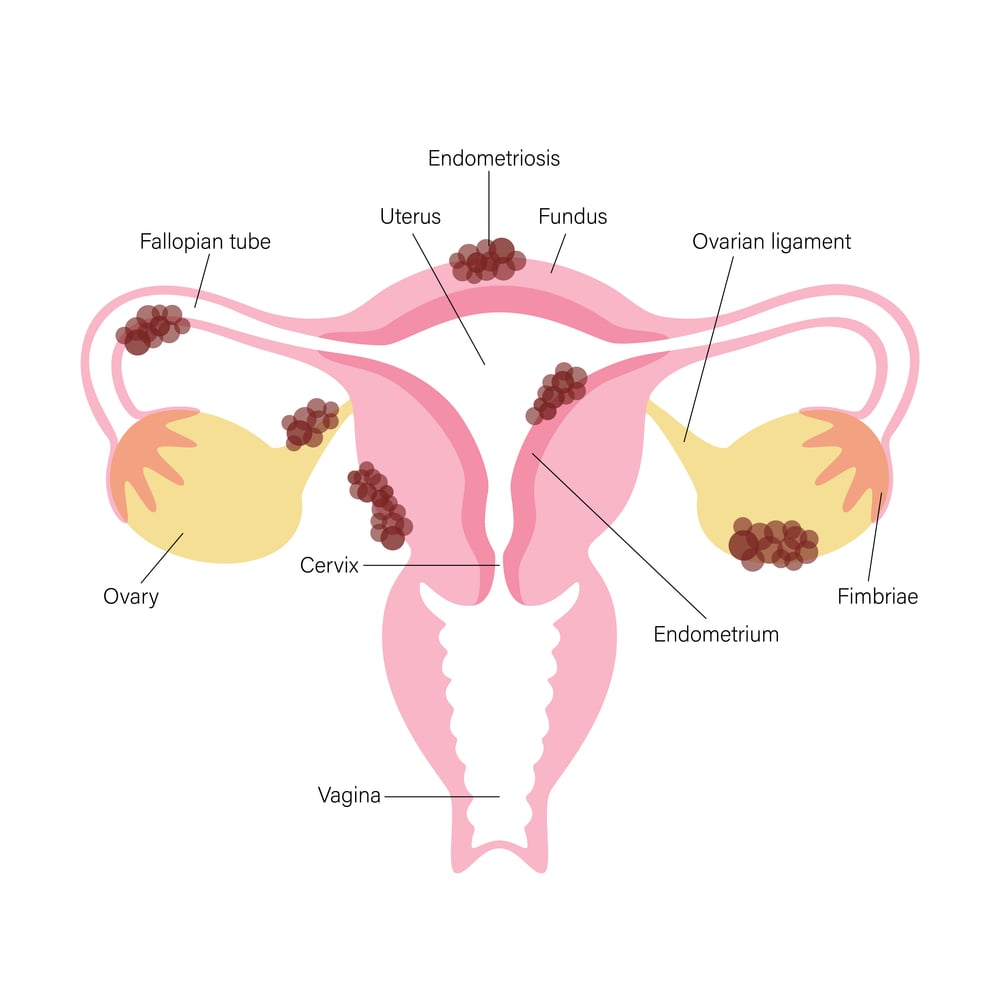
When adhesions form in the pelvic region, they can trigger a spectrum of symptoms depending on which organs and tissues are involved. For instance, if the ovaries become ensnared in scar tissue or adhere to the pelvic walls, the presence of an ovarian cyst can stretch these adhesions, leading to a painful, tugging sensation. Conversely, if the intestines are affected by adhesions, individuals may experience intense cramping pains due to restricted movement of the bowels. In severe cases where a segment of the bowel is constricted by an adhesion, partial or complete bowel obstruction can occur, resulting in severe pain, nausea, vomiting, constipation, or diarrhea.
In the most severe instances of adhesions, the pelvic region can become immobilized by dense scar tissue, effectively fusing organs together. This can manifest as the bladder adhering to the uterus, the uterus connecting to the large bowel, or the ovaries and fallopian tubes becoming intertwined with the bowel, pelvic sidewalls, and uterus. In rare scenarios, severe adhesions can completely envelop the abdominal cavity, distorting pelvic anatomy to the extent that surgeons must painstakingly dissect through layers of scar tissue to identify organs.
Navigating adhesions can be challenging, but with the right expertise and support, patients can find relief and restoration of their quality of life.
How are Adhesions Treated?
When it comes to pelvic adhesions, there currently aren’t any non-invasive medications or treatments capable of breaking them down or eliminating them. However, techniques like massage and physical therapy may offer some relief by helping to stretch and loosen adhesions, thereby mobilizing organs. Despite these efforts, surgery remains the primary method for effectively removing adhesions.
Yet, surgery itself poses a challenge as it can contribute to the formation of new adhesions. This underscores the importance of entrusting this procedure to highly skilled professionals equipped with specialized techniques to minimize the risk of recurrence.
In the case of patients grappling with severe endometriosis, the presence of significant scar tissue and adhesions is often a consequence of the inflammatory disease process. To prevent the recurrence of these adhesions post-surgery, it's imperative to thoroughly remove all areas affected by the disease. Simply addressing the adhesions without addressing the underlying disease can lead to continued inflammation and the formation of new adhesions over time. Once the disease has been completely excised, various measures can be implemented to reduce the likelihood of post-operative adhesions.
Adhesion Surgery Techniques
No matter the underlying cause of your adhesions, there are several techniques available to address them, aiming to remove scar tissue, restore pelvic anatomy, alleviate associated pain, and prevent recurrence.
Adhesiolysis
Adhesiolysis serves as the initial step in adhesion surgery. This involves delicately dissecting structures that have become fused due to adhesions. Performing adhesiolysis requires advanced laparoscopic surgical skills and a deep understanding of pelvic anatomy to ensure the safe removal of all adhesions and scarring without causing harm to surrounding structures.
Following adhesiolysis, patients often have multiple areas of raw tissue. If left untreated, adjacent structures may adhere to these raw areas, leading to the formation of new adhesions. Typically, this process occurs within the first hours and days following surgery, with newly formed adhesions potentially thickening and tightening in the months that follow. While this natural healing response is the body's way of addressing injury, some individuals may be more prone to forming scar tissue and adhesions than others.
Adhesion Barriers
Following adhesiolysis, the placement of adhesion barriers over raw tissue areas can be instrumental in preventing recurrence and facilitating healing. These barriers are designed to safeguard vulnerable tissue during the healing process. While barriers that are used are biodegradable and dissolve over time, others do not and have to be removed in a second-look laparoscopy. Securing a non-absorbable barrier in place be intricate and may sometimes be avoided by physicians who lack specialization in endometriosis surgery.

One notable barrier, Gore-Tex, has shown promising outcomes for pregnancy in Dr. Yeung's practice in patients with infertility who have required cystectomy for an endometriosis.
Ovarian Suspension
In cases where adhesions tether the ovaries to nearby structures, a temporary solution involves suspending the ovaries by suturing them away from raw surfaces. This maneuver helps prevent re-adhesion in their previous position. Typically, these sutures dissolve within weeks after the initial surgery, allowing for a smooth transition of ovaries to normal positioning without adhesion.
Offering Hope for Those Affected by Adhesion-Related Pain
If you find yourself grappling with adhesion-related pain, it's important to know that there is hope. Expert laparoscopic removal of adhesions, coupled with the strategic application of adhesion barriers, offers promising avenues for long-term relief and recurrence prevention.
Related Posts